Core Question: Why is Titanium Alloy the First Choice for Medical Parts? How to Balance Safety and Precision in Customization?

I. Medical Titanium Alloy: “Life Compatibility” Determined by Material Properties
The strict requirements of medical equipment parts for materials make titanium alloy an irreplaceable choice. This metal, with a density of only 4.5g/cm³, can achieve the dual value of “safe load-bearing” and “biological integration” in the complex physiological environment of the human body. Its core advantages are reflected in three dimensions:
- Biocompatibility: A “Friendly Partner” of the Human Body
A dense TiO₂ oxide film can naturally form on the surface of titanium alloy, which effectively blocks the precipitation of metal ions and avoids immune rejection reactions. Medical-grade titanium alloy must pass the ISO 10993 biocompatibility test, among which the cytotoxicity must reach Grade 0 (cell survival rate ≥70%) and the incidence of sensitization reactions is less than 8%. For example, TC4ELI (Ti-6Al-4V ELI) further improves biological safety by reducing the oxygen content to ≤0.13%, making it the first choice for load-bearing implants such as artificial joint stems.
- Mechanical Matching: A “Performance Substitute” for Bones
The strength-to-weight ratio of titanium alloy is much higher than that of steel and aluminum alloy, with a tensile strength of over 1000MPa. At the same time, its elastic modulus is closer to that of human bones (about 80GPa), which can reduce the bone resorption problem caused by the “stress shielding effect”. The new Ti-13Nb-13Zr alloy reduces the elastic modulus by 30% through vanadium-free design, reducing the postoperative bone resorption rate of spinal fusion cages by 50% and solving the problem of mechanical mismatch between traditional materials and bones.
- Environmental Stability: A “Tolerator” of Harsh Conditions
In corrosive environments such as body fluids and disinfectants, titanium alloy can work stably for a long time without additional anti-corrosion treatment. Electrochemical tests show that its corrosion current density can be controlled at ≤0.1μA/cm², and it can withstand 121℃ moist heat sterilization and γ-ray disinfection with a performance retention rate of over 95%, perfectly adapting to the repeated disinfection needs of medical equipment.
II. Full Customization Process: A 10-Step Compliant Closed Loop from Demand to Delivery
The customization of medical titanium alloy parts is by no means a simple “processing according to drawings”, but a full-chain quality control covering “design-materials-processes-testing”. The core process includes 10 key links:
(I) Demand Definition: Accurate Matching with Clinical Scenarios
First, it is necessary to clarify the core parameters of the part, such as the use environment (implanted in the body / equipment), mechanical requirements (load-bearing/non-load-bearing), and disinfection method (ethylene oxide/high-temperature and high-pressure). For example, orthopedic bone plates need to meet the requirements of tensile strength ≥895MPa and elongation ≥10%, while the coaxiality of lens holders for imaging equipment requires ≤±0.001mm. Different requirements directly determine the subsequent material and process selection.
(II) Material Selection: Dual Locking of Grade and Standard
Medical titanium alloy must strictly comply with international standards, and the application scenarios of common grades are clearly differentiated:
- Pure Titanium Series (TA1/TA2): Oxygen content ≤0.20%, suitable for non-load-bearing parts such as dental abutments and skull repair meshes, in line with ASTM F67 standards;
- TC4 Alloy (Ti-6Al-4V): Tensile strength ≥895MPa, suitable for surgical instruments and ultrasonic scalpel heads, requiring compliance with ISO 5832-3:2021 specifications;
- TC4ELI (Grade 23): Ultra-low interstitial type, oxygen content ≤0.13%, fracture elongation increased to ≥18%, specially designed for long-term load-bearing implants such as hip joint stems;
- New Vanadium-Free Alloy (Ti-13Nb-13Zr): Avoids the risk of vanadium ion toxicity, with Nb₂O₅ in the oxide film, suitable for long-term implants such as cardiovascular stents.
The purchase of materials must be accompanied by the original Material Test Certificate (MTC), and the purity of components must be verified by ICP-OES spectral analysis to ensure that the content of impurity elements (iron, nitrogen) meets medical-grade requirements.
(III) Process Implementation: Overcoming the Processing Difficulties of Titanium Alloy
Titanium alloy has poor thermal conductivity (only 1/5 of steel) and large elastic deformation, which puts forward extreme requirements for processing technology. The core technical paths include:
- Precision Machining
Ultra-precision CNC lathes with spindle runout ≤0.0005mm and 5-axis machining centers with positioning accuracy of ±0.001mm are used. Through centerless grinding with CBN grinding wheels, the diameter tolerance is controlled within ±0.01mm. When processing TC4 bone plates, low-temperature cutting fluid (-5℃) is used to reduce cutting heat, avoid dimensional deviations caused by tool wear, and complete curved surface processing in one clamping to reduce positioning errors.
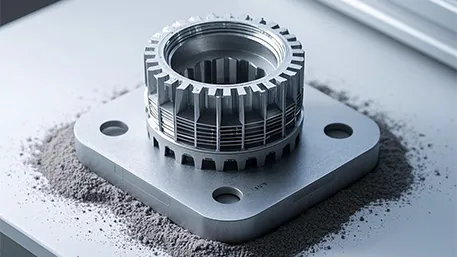
- Additive Manufacturing (3D Printing)
Selective Laser Melting (SLM) technology has become the first choice for complex structural parts, which can directly print personalized implants such as trabecular prostheses based on CT data. By adjusting the laser power (150-300W) and scanning speed (800-1200mm/s), the grain morphology is controlled—high power and low speed form coarse columnar grains (high strength), while low power and high speed obtain fine equiaxed grains (high toughness). The prosthesis developed by the First Affiliated Hospital of Shandong First Medical University using this technology has shortened the osseointegration cycle to 8 weeks and reduced the postoperative secondary collapse rate to 0.3%.
- Surface Functionalization Treatment
Surface characteristics are customized according to different application needs: implants use sandblasting and acid etching (SLA) to form a rough surface with Ra 0.8-1.5μm to promote osteocyte adhesion; parts of testing equipment achieve a mirror finish with Ra ≤0.1μm through electrolytic polishing to avoid sample residue; suture anchors undergo picosecond laser microtexturing treatment, and the surface groove array increases the pull-out force by 21%.
(IV) Quality Testing: Full-Dimensional Verification from Microcosm to Macrocosm
Medical parts need to pass a triple testing closed loop of “materials-processes-finished products”, and the key items include:
- Physical and Chemical Testing: Ultrasonic Testing (UT) is used in accordance with AMS 2631B standards to ensure internal defects ≤Φ0.8mm equivalent flat-bottomed holes; tensile tests verify tensile strength and elongation, and fatigue tests simulate 10⁷ cycles of load cycling;
- Biocompatibility: Cytotoxicity tests (MTT method) and sensitization tests are carried out in accordance with ISO 10993; implants need to pass the 28-day rabbit muscle implantation test, with a bone-implant contact rate (BIC) ≥60%;
- Cleanliness and Sterilization: The surface cleanliness must reach ISO 8573-1 Class 1, the residual amount after ethylene oxide sterilization ≤4μg/cm², and the Sterility Assurance Level (SAL) ≥10⁻⁶.
III. Typical Application Scenarios: Technical Parameters Determine Clinical Value
Different medical equipment have significantly different performance requirements for titanium alloy parts, and accurate matching is the core of customization:
- Implantable Parts
Artificial joint stems use TC4ELI alloy, and the grain size is refined to ≤Grade 5 through multi-directional forging, with compression set ≤15% (150℃×22h) to ensure a service life of more than 15 years; spinal fusion cages use Ti-13Nb-13Zr alloy, with an elastic modulus of 80GPa, which improves the mechanical matching with vertebral bodies by 40% and the postoperative pain relief rate reaches 92%.
- Testing Equipment Parts
The TC4 detection chamber of biochemical analyzers needs to achieve an inner diameter tolerance of ±0.003mm and roundness ≤0.0005mm through 5-axis milling, and the inner wall is electrolytically polished to ensure a sample detection error ≤±0.1%; the optical lens holder of immunoassay equipment undergoes anodizing treatment (film thickness 5-8μm), with an installation deviation ≤±0.001mm and imaging distortion controlled within 0.05%.
- Surgical Instrument Parts
Ultrasonic scalpel heads use special TC4 wire rods, and after annealing at 730℃, the tensile strength reaches 1050-1100MPa and the elastic modulus ≥130GPa, which can withstand high-frequency vibration of 5000 times per minute without fatigue fracture; laparoscopic forceps heads achieve a weld penetration ≥0.5mm through laser welding, and the pressure drop is ≤0.001MPa during the 0.3MPa pressure holding test for 30 minutes in the tightness test.
IV. Customization Selection Guide: Key Points for Avoiding Pitfalls and Decision-Making Basis
- Three Principles of Material Selection
- For load-bearing parts, TC4ELI (fatigue resistance) is preferred; for non-load-bearing parts, TA2 (low cost) is preferred; for long-term implants, vanadium-free alloys (Ti-13Nb-13Zr) are preferred;
- For complex structures (such as porous prostheses), SLM 3D printing is a must; for high-precision regular parts, 5-axis machining is selected;
- Parts in contact with body fluids need additional electrochemical corrosion tests to ensure the corrosion current density ≤0.1μA/cm².
- Core Standards for Service Provider Selection
- Qualification Certification: Must have ISO 13485 medical device quality management system certification; implant production must pass FDA 21 CFR 888.3 registration;
- Equipment Capability: Verify the spindle speed of 5-axis machining centers (≥40000r/min), laser accuracy of SLM equipment (±0.02mm), and testing equipment (coordinate measuring machine accuracy ≥0.0005mm);
- Case Experience: Priority is given to manufacturers with delivery records of similar products; for example, orthopedic parts need to provide clinical application data, and testing equipment parts need to have accuracy compliance reports.
- Cost and Cycle Balance Strategy
For standard parts, the “batch prefabrication + personalized processing” model is adopted, shortening the cycle by 30%; for complex parts, process optimization is carried out through simulation to reduce trial-and-error costs—an enterprise used the SLM adaptive support algorithm developed by Shanghai Jiao Tong University to reduce the post-processing cost of hip cups by 50%.
Disclaimer
- All information, opinions, and data contained in this article are for the purpose of information transmission only and do not constitute any advice on investment, transactions, law, medical care, or other matters.
- The content of the article is compiled based on public information or created based on the author’s personal understanding. Although every effort is made to ensure accuracy, it does not guarantee the completeness, accuracy, and timeliness of the information, nor does it bear any responsibility for any losses caused by the use of the content of this article.
- If the article involves third-party opinions, pictures, data, and other content, the copyright belongs to the original author. In case of infringement, please contact us for deletion.
- Readers should make independent decisions based on their actual situation and combined with professional opinions. The user shall bear all consequences arising from the use of the content of this article.
A senior engineer who has been engaged in medical titanium alloy processing technology for 15 years, leading the research and development of a series of products such as 3D-printed titanium alloy bone implants and ultra-precision testing equipment parts.